Oxalates and Autoimmunity: The Hidden Connection to Microbial Imbalance
- Dr. Brendan McLaughlin
Share
- Oxalates come from both dietary sources AND microbial production inside the body
- Specific microorganisms (Candida, Aspergillus, and certain parasites) are significant oxalate producers
- Oxalates can trigger autoimmunity through tissue damage, molecular mimicry, intestinal permeability, and mitochondrial dysfunction
- Testing for both oxalates AND microbial markers is essential for comprehensive treatment
- Addressing the microbial component is critical for patients who don’t respond to dietary interventions alone
What Are Oxalates and How Do They Contribute to Autoimmunity?
Specific Autoimmune Conditions Linked to Oxalate Accumulation
Research and clinical observation have shown that oxalate accumulation may play a role in several specific autoimmune conditions:
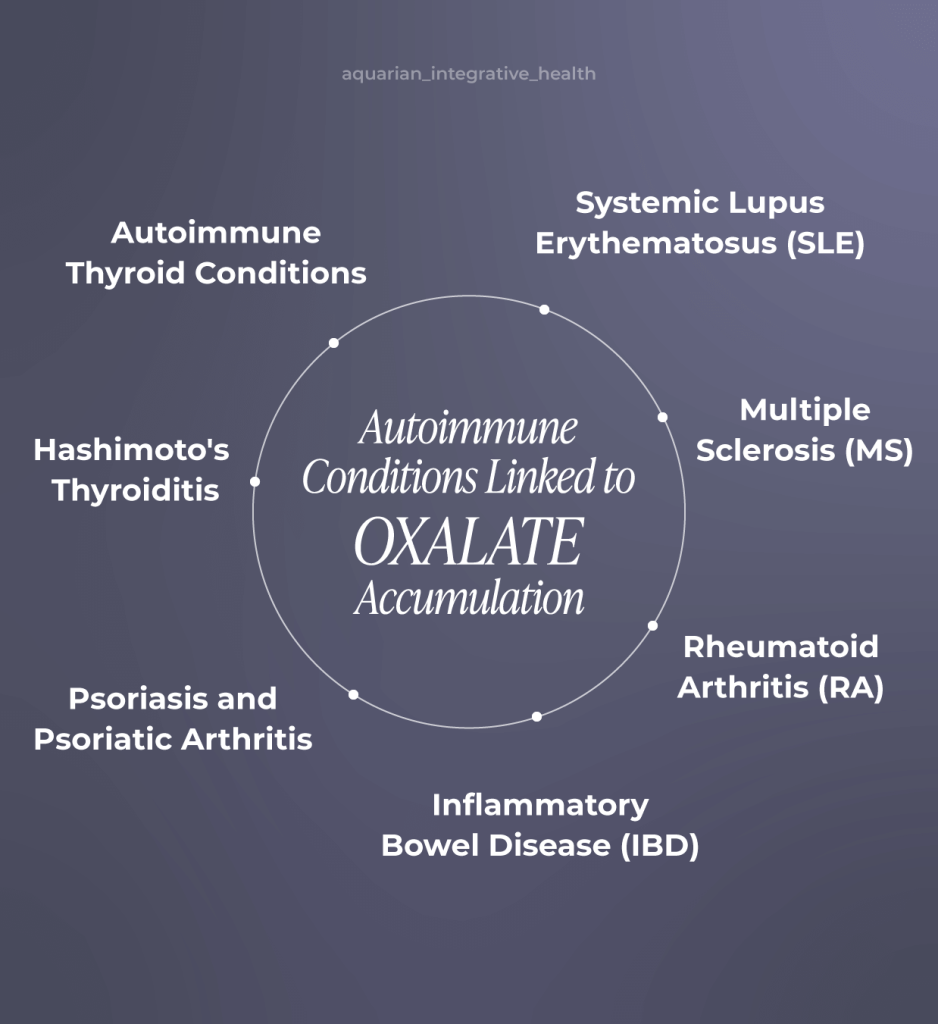
- Multiple Sclerosis (MS): Studies have found oxalate crystal deposits in brain tissues of MS patients. These deposits can trigger neuroinflammation and contribute to demyelination processes. The mitochondrial dysfunction caused by oxalates may accelerate neurodegeneration.
- Rheumatoid Arthritis (RA): Oxalate crystals have been detected in synovial fluid and joint tissues of RA patients. These crystals can activate the NLRP3 inflammasome pathway, contributing to joint inflammation and cartilage degradation.
- Hashimoto’s Thyroiditis: Clinical observations suggest that oxalate accumulation in thyroid tissue may trigger antibody responses against thyroid peroxidase (TPO) and thyroglobulin through molecular mimicry mechanisms.
- Systemic Lupus Erythematosus (SLE): The systemic nature of SLE makes it particularly susceptible to widespread oxalate crystal deposition, potentially contributing to multi-organ inflammation.
- Inflammatory Bowel Disease (IBD): Oxalates can directly damage intestinal mucosa, exacerbating intestinal permeability issues already present in Crohn’s disease and ulcerative colitis.
- Psoriasis and Psoriatic Arthritis: Skin manifestations of oxalate accumulation have been documented, potentially contributing to the characteristic skin lesions in psoriasis.
- Autoimmune Thyroid Conditions: Both Graves’ disease and Hashimoto’s thyroiditis patients have shown improvement with oxalate reduction protocols in clinical settings.
Beyond Food Sources - The Overlooked Oxalate Equation
High-Oxalate Foods: The Usual Suspects
- Spinach (raw, 1 cup): 750mg
- Swiss chard (cooked, 1 cup): 102mg
- Beet greens (cooked, 1 cup): 91mg
- Rhubarb (cooked, 1 cup): 86mg
- Almonds (1/4 cup): 122mg
- Almond butter (2 Tbsp): 79mg
- Almond milk (1 cup): 65mg
- Cashews (1/4 cup): 49mg
- Potatoes with skin (1 medium): 97mg
- Sweet potatoes (1 medium): 56mg
- Beets (1/2 cup): 76mg
- Navy beans (1/2 cup): 52mg
- Dark chocolate (1 oz): 65mg
- Black tea (8 oz): 55mg
- Kale (raw, 1 cup): 36mg
- Peanuts (1/4 cup): 27mg
- Peanut butter (2 Tbsp): 25mg
- Quinoa (1/2 cup cooked): 48mg
- Blueberries (1/2 cup): 33mg
- Blackberries (1/2 cup): 25mg
- Raspberries (1/2 cup): 22mg
- Okra (1/2 cup): 26mg
- Celery (1 cup): 19mg
- Dried figs (3 medium): 24mg
- Sesame seeds (1 Tbsp): 35mg
- Brown rice (1/2 cup): 24mg
The Microbial Connection: When Microorganisms Produce Oxalates
What many practitioners and patients don’t realize is that oxalates don’t just come from food. A wide variety of microorganisms in our body can actually produce oxalates independently of our diet. This is a critical piece of the puzzle when addressing oxalate-related health issues.
- Candida albicans
- The most common fungal pathogen in humans
- Produces significant amounts of oxalates as metabolic byproducts
- Often proliferates after antibiotic use or with high-sugar diets
- Clinical studies show direct correlation between Candida overgrowth and urinary oxalate levels
- Aspergillus niger
- One of the most prolific oxalate producers among all microorganisms
- Can colonize the respiratory tract and sinuses
- Studies show it can produce up to 20x more oxalates than other Aspergillus species
- Often found in patients with chronic sinusitis and respiratory conditions
- Cryptosporidium species
- Parasitic infection strongly associated with hyperoxaluria
- Studies show altered oxalate metabolism during infection
- Often missed in conventional parasitology testing
- Frequently found in patients with unexplained oxalate issues despite dietary changes
- Other Candida species
- Candida glabrata and Candida tropicalis
- Significant oxalate producers, though typically less prevalent than C. albicans
- Often co-occur with Candida albicans in systemic fungal overgrowth
- Aspergillus fumigatus
- Common cause of respiratory infections
- Produces oxalates as part of its virulence mechanisms
- More commonly problematic in immunocompromised individuals
- Pseudomonas aeruginosa
- Opportunistic bacterial pathogen
- Produces oxalates through alternative metabolic pathways
- Often resistant to conventional antimicrobial treatments
- Frequently found in chronic respiratory and urinary tract infections
- Giardia lamblia
- During giardiasis, patients show increased oxalate levels
- Disrupts normal gut flora balance, reducing oxalate-degrading species
- May persist chronically in some patients despite treatment
- Blastocystis hominis
- Some strains associated with increased oxalate levels in patients
- Connection to irritable bowel syndrome where oxalate issues are sometimes observed
- Controversial parasite with varying pathogenicity between strains
- Penicillium species
- Penicillium chrysogenum and Penicillium oxalicum
- Environmental fungi that can colonize the GI tract
- Notable oxalate producers, though less commonly found than Candida/Aspergillus
- Streptomyces species
- Several soil bacteria in this genus that can colonize the gut
- Produce oxalates as secondary metabolites
- Lactobacillus species
- Some strains of these otherwise beneficial bacteria can produce oxalates under certain conditions
- Highlights the importance of strain-specific probiotic selection
- Bifidobacterium species
- Some species can produce oxalates while others degrade them
- Strain-specific effects important in probiotic therapy
- Helminth parasites
- Including Schistosoma and Ascaris species
- May contribute to oxalate issues through multiple mechanisms
- More common in individuals with travel history to endemic regions
- Glyoxylate cycle – In this pathway microbes use when in glucose-limited environments, the enzyme glyoxylate oxidase directly converts glyoxylate (a two-carbon compound) to oxalate
- Krebs cycle intermediates – The Krebs cycle is the central metabolic pathway for aerobic organisms. Some microbes have enzymatic pathways that convert malate and succinate (Krebs cycle intermediates) into precursors that eventually form oxalate.
- Glycolate pathway – This pathway that microbes use in high oxygen environments involves the conversion of glycolate to oxalate.
- Ascorbic acid metabolism – Some microorganisms (especially Aspergillus) can metabolize ascorbic acid (vitamin C) through pathways that generate oxalate as an end product. This pathway explains why high-dose vitamin C supplementation can increase oxalate levels in susceptible individuals.
- Direct production – Many microbes directly synthesize oxalates as metabolic byproducts
- Indirect mechanisms:
- Damaging intestinal mucosa, altering oxalate absorption
- Disrupting the gut microbiome, reducing populations of oxalate-degrading bacteria
- Causing inflammation that alters normal metabolic processes
- Increasing intestinal permeability, allowing greater oxalate absorption
- Creating localized pH changes that affect oxalate solubility
- Secondary effects:
- Inducing oxidative stress that can increase endogenous oxalate production
- Metabolizing host nutrients in ways that generate oxalate precursors
- Chronic fungal overgrowth
- Small intestinal bacterial overgrowth (SIBO)
- Post-antibiotic dysbiosis
- Chronic parasitic infections
- Immunocompromised states where opportunistic infections flourish
How Oxalates Trigger Autoimmune Responses
- Tissue Damage and Inflammation: When oxalate crystals form in tissues, they can cause physical damage and trigger localized inflammation.
- Molecular Mimicry: The immune response to oxalate crystals may sometimes cross-react with the body’s own tissues through a process called molecular mimicry, potentially triggering autoimmune reactions.
- Increased Intestinal Permeability: Oxalate crystals can damage the intestinal lining, contributing to “leaky gut,” which allows larger molecules to enter the bloodstream and potentially trigger immune responses.
- Disruption of Mitochondrial Function: Oxalates can interfere with cellular energy production in mitochondria, leading to oxidative stress and cellular dysfunction that may contribute to autoimmune processes.
The Vicious Cycle: Infection, Oxalates, and Immune Dysregulation
- Microbial overgrowth produces oxalates
- Oxalates damage tissues and trigger inflammation
- Inflammation alters immune function and gut permeability
- Increased gut permeability allows more microbes to translocate
- More inflammation leads to further immune dysregulation
Clinical Approaches to Breaking the Cycle
- Identify and address underlying infections or dysbiosis
- Support detoxification pathways to help clear accumulated oxalates
- Support healthy oxalate metabolism with calcium, magnesium, and vitamin B6
- Gradually reduce dietary oxalates (sudden reduction can cause “dumping” symptoms)
- Restore beneficial gut bacteria that can degrade oxalates, particularly Oxalobacter formigenes
Testing for Oxalates: The Power of Organic Acid Testing
- Oxalic Acid: Direct measurement of oxalate levels in the urine. Elevated levels can indicate either high dietary intake, increased endogenous production, or impaired oxalate metabolism.
- Glyceric Acid: Elevated levels may indicate issues with glyoxylate metabolism, which can lead to increased oxalate production.
- Glycolic Acid: Another metabolite in the glyoxylate pathway, elevated levels can suggest increased endogenous oxalate production.
- Arabinose: Elevated levels suggest Candida overgrowth, which can produce oxalates
- Tartaric Acid: Often elevated with certain fungal infections
- Citramalic Acid: Associated with certain bacterial imbalances
- Furan compounds: Indicators of intestinal dysbiosis
- Elevated Oxalates with Normal Microbial Markers: May suggest primarily dietary sources or genetic factors affecting oxalate metabolism (such as Primary Hyperoxaluria).
- Elevated Oxalates with Elevated Fungal Markers: Strongly suggests fungal contribution to oxalate burden, requiring targeted antifungal therapies along with oxalate reduction.
- Elevated Oxalates with Multiple Dysbiosis Markers: Indicates complex gut ecology issues contributing to oxalate problems, requiring comprehensive gut restoration.
- Moderately Elevated Oxalates with Mitochondrial Dysfunction Markers: May indicate that oxalates are impacting cellular energy production, potentially contributing to fatigue and chronic inflammation.
- Autonomic Response Testing: to identify precisely which foods and microbes are triggering oxalate fueled inflammation
- Comprehensive stool analysis: To identify specific microbial imbalances
- Inflammatory markers: To assess the degree of systemic inflammation
- Autoimmune panels: To evaluate for specific autoimmune markers that may be related to oxalate burden
Conclusion
References
- Knight J, Madduma-Liyanage K, Mobley JA, Assimos DG, Holmes RP. Ascorbic acid intake and oxalate synthesis. Urolithiasis. 2016;44(4):289-297. doi:10.1007/s00240-016-0868-7
- Abratt VR, Reid SJ. Oxalate-degrading bacteria of the human gut as probiotics in the management of kidney stone disease. Adv Appl Microbiol. 2010;72:63-87. doi:10.1016/S0065-2164(10)72003-7
- Jayaram N, Sharma RK, Nagarathna R, Nagendra HR. Role of fungal oxalates in the formation of calcium oxalate kidney stones in Hyperoxaluria. Int Urol Nephrol. 2021;53(4):697-706. doi:10.1007/s11255-020-02695-5
- Peck AB, Canales BK, Nguyen CQ. Oxalate-degrading microorganisms or oxalate-degrading enzymes: Which is the future therapy for enzymatic dissolution of calcium-oxalate uroliths in recurrent stone disease? Urolithiasis. 2016;44(1):45-50. doi:10.1007/s00240-015-0797-x
- Al KF, Bisanz JE, Reid G, Burton JP. The microbiome and oxalate nephrolithiasis: a novel application of microbial ecology. World J Urol. 2019;37(9):1741-1746. doi:10.1007/s00345-018-2550-x
- Ticinesi A, Nouvenne A, Di Gregorio L, et al. Microbiome-metabolome correlations in kidney stone patients with and without Randall’s plaque. Metabolites. 2021;11(8):506. doi:10.3390/metabo11080506
- Banwo K, Akinde SB, Andriamihaja M, et al. Yeasts and moulds as efficient consumers of oxalate: Impact on intestinal oxalate homeostasis. mBio. 2022;13(2):e03543-21. doi:10.1128/mbio.03543-21
- Talham DR, Backov R, Benitez IO, et al. Role of microorganisms in kidney stone formation. In: ACS Symposium Series. Vol 1438. American Chemical Society; 2020:163-181. doi:10.1021/bk-2020-1348.ch009
- Van der Hoeven TA, Hollander JC, Lefeber DJ, et al. Oxalate-metabolizing bacteria in the human gut: a potential therapeutic target for hyperoxaluria. Microbiome. 2022;10(1):38. doi:10.1186/s40168-022-01228-9
- Liebman M, Al-Wahsh IA. Probiotics and other key determinants of dietary oxalate absorption. Adv Nutr. 2011;2(3):254-260. doi:10.3945/an.111.000414
- Salem F, Kindt R, Ahmedna M, et al. Oxalate nephropathy and autoimmunity: an overlooked connection. Front Immunol. 2023;14:1112234. doi:10.3389/fimmu.2023.1112234
- Miller AW, Choy D, Penniston KL, Lange D. Inhibition of urinary stone disease by a multi-species bacterial network ensures proper oxalate homeostasis. Kidney Int. 2019;96(1):180-188. doi:10.1016/j.kint.2019.02.012
- Mulay SR, Anders HJ. Crystal nephropathies: mechanisms of crystal-induced kidney injury. Nat Rev Nephrol. 2017;13(4):226-240. doi:10.1038/nrneph.2017.10
- Vojdani A, Rahimian P, Kalhor H, Mordechai E. Immunological cross reactivity between Candida albicans and human tissue. J Clin Lab Immunol. 1996;48(1):1-15.
- Chen X, Dai Y, Kong X, et al. Molecular mechanisms of crystal-induced inflammation in gouty arthritis and calcium crystal diseases. Front Immunol. 2021;12:700172. doi:10.3389/fimmu.2021.700172
- Nazzal L, Puri S, Goldfarb DS. Enteric hyperoxaluria: an important cause of end-stage kidney disease. Nephrol Dial Transplant. 2016;31(3):375-382. doi:10.1093/ndt/gfv005
- Canales BK, Hatch M. Oxalobacter formigenes colonization normalizes oxalate excretion in a gastric bypass model of hyperoxaluria. Surg Obes Relat Dis. 2017;13(7):1152-1157. doi:10.1016/j.soard.2017.03.014
- Ticinesi A, Milani C, Guerra A, et al. Understanding the gut-kidney axis in nephrolithiasis: an analysis of the gut microbiota composition and functionality of stone formers. Gut. 2018;67(12):2097-2106. doi:10.1136/gutjnl-2017-315734
- Hatch M, Freel RW. The roles and mechanisms of intestinal oxalate transport in oxalate homeostasis. Semin Nephrol. 2008;28(2):143-151. doi:10.1016/j.semnephrol.2008.01.007
- Mantovani V, Trinchieri A, Castelnuovo C, Romanò AL, Pisani E. Reconstructive surgery for complex renal stones. Arch Ital Urol Androl. 2019;91(1):25-29. doi:10.4081/aiua.2019.1.25
JUST LAUNCHED
The Autoimmune Revival Method™
The same breakthrough that saved my wife has now helped hundreds of patients break free from chronic fatigue, pain, and inflammation, naturally and permanently.
A Results-Driven Approach to Feeling your Best
Traditional medicine often stops at symptom management, leaving the real problem untreated. Our science-backed approach uncovers the true root cause, treating the whole person to restore your energy, balance, and long-term health.