Mycotoxins and Autoimmunity: Understanding the Hidden Triggers in Your Food
- Dr. Brendan McLaughlin
Share
What Are Mycotoxins?
How Mycotoxins Trigger Autoimmunity
1. Intestinal Hyperpermeability ("Leaky Gut")
- Increased exposure of the immune system to previously sequestered proteins
- Activation of pattern recognition receptors that stimulate inflammatory cascades
- Enhanced presentation of food antigens to immune cells, potentially establishing molecular mimicry
- Chronic stimulation of the immune system at the gut lining (mucosa)
2. Molecular Mimicry
3. Immune System Dysregulation
- T-cell Imbalance: T-cells are specific types of white blood cell that play a central role in our immune systems. Mycotoxins like aflatoxin and trichothecenes can alter the balance between different T-cell populations (Th1, Th2, Th17, and Treg cells). This imbalance is particularly relevant for autoimmunity, as a shift away from regulatory T-cells (Tregs) toward inflammatory Th17 cells is a hallmark of many autoimmune conditions.
- Dendritic Cell Activation: Mycotoxins can activate dendritic cells, the primary antigen-presenting cells that instruct T-cells whether to mount an immune response. When inappropriately activated, dendritic cells can present self-antigens to T-cells, potentially initiating autoimmune reactions.
- Cytokine Disruption: Mycotoxins also can alter cytokine production (small proteins that act as chemical messengers in the body within the immune system), often increasing pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) while decreasing anti-inflammatory ones (IL-10). This inflammatory environment promotes tissue damage and further immune dysregulation.
- Inflammasome Activation: Certain mycotoxins activate the NLRP3 inflammasome, a protein complex that triggers the release of IL-1β and IL-18 cytokines which are strongly associated with autoimmune conditions like rheumatoid arthritis and multiple sclerosis.
4. Toxic Burden and Cellular Stress
- Oxidative Stress: Mycotoxins dramatically increase reactive oxygen species (ROS) production while depleting antioxidant defenses like glutathione. This oxidative stress can damage cellular proteins, creating neo-antigens the immune system may recognize as foreign. Oxidative stress can also modify DNA, potentially exposing nuclear antigens that can trigger autoantibody formation and activate stress-response pathways that enhance inflammatory signaling.
- Mitochondrial Dysfunction: Many mycotoxins directly impair mitochondrial function, leading to decreased energy production and increased oxidative stress. This is important because mitochondrial dysfunction is increasingly recognized as a factor in autoimmune conditions like lupus and rheumatoid arthritis.
- Impaired Detoxification: Mycotoxins can readily overwhelm and impair the body’s detoxification pathways which can lead to accumulation of toxins and metabolic waste within the body and as a result prolong exposure to immune-stimulating compounds. Impaired detoxification can also deplete key nutrients essential for immune regulation. The net result of impaired detoxification is increased inflammation throughout the body which can precipitate autoimmunity.
5. Endocrine Disruption
6. Microbiome Disruption
As you can see, through various mechanisms mycotoxins can disrupt our immune systems leading us down a path towards autoimmunity or exacerbate pre-existing autoimmune conditions. In my clinical experience, remediating mycotoxin exposure in patients with autoimmune conditions leads to significant symptom improvement and wellbeing.
Key Types of Mycotoxins and Their Impact
1. Aflatoxins
- Corn and corn products
- Peanuts and peanut butter
- Tree nuts (especially pistachios and almonds)
- Cottonseed
- Spices (particularly paprika and chili)
- Dried fruits
- Milk (from animals consuming contaminated feed)

- Impair protein synthesis
- Suppress immune function
- Contribute to oxidative stress
- Interfere with gut barrier function
- Disrupt the microbiome
2. Ochratoxins
- Coffee beans
- Wine and grape juice
- Cereals (wheat, barley, oats)
- Dried fruits (especially raisins)
- Cocoa and chocolate
- Spices
- Beer
- Aged and fermented meats

- Nephrotoxicity (kidney damage)
- Immunosuppressive effects
- Neurotoxicity
- Potential teratogenic effects (birth defects)
- Disruption of mitochondrial function
- Promotion of oxidative stress
- Inhibition of protein synthesis
- Disruption of calcium homeostasis
3. Fumonisins
- Corn and corn-based products (cornmeal, corn flour, corn chips)
- Rice
- Sorghum
- Occasionally in beer (from contaminated grains)

- Neural tube defects
- Liver damage
- Kidney toxicity
- Esophageal cancer (in regions with high exposure)
- Immune system dysfunction
- Intestinal barrier damage
- Altered cytokine production
4. Trichothecenes
- Wheat and wheat products (bread, pasta)
- Barley
- Corn
- Oats
- Rye
- Animal products from animals that are fed the above

- Potent inhibitor of protein synthesis
- Gastrointestinal distress (nausea, vomiting, diarrhea)
- Immune system alterations
- Disruption of gut barrier function
- Neurological effects (fatigue, headaches)
- Hormonal disruption
- Chronic migraines
- Overgrowth of saccharomyces cerevisiae
5. T-2 Toxin and HT-2 Toxin
- Oats
- Barley
- Wheat
- Rye
- Corn
- Rice

- Extremely potent inhibitors of protein synthesis
- Skin irritation and inflammation
- Digestive system damage
- Blood cell depletion
- Immune suppression
- Cell death in various tissues
6. Zearalenone
- Corn
- Wheat
- Barley
- Oats
- Sorghum
- Animal products (from livestock fed contaminated grains)

- Bind to estrogen receptors
- Disrupt hormonal balance
- Cause reproductive issues
- Contribute to breast tissue changes
- Affect thyroid function
- Interfere with immune regulation
7. Patulin
- Apple juice and apple products
- Pears
- Berries
- Other fruits with brown rot

- Gastrointestinal inflammation
- Immunotoxicity
- Neurotoxicity
- DNA damage
- Disruption of the gut microbiome
- Potential developmental effects
8. Citrinin
- Rice and rice products
- Wheat
- Corn
- Barley
- Oats
- Fermented foods (some cheeses, sake)
- Fruits (particularly red fruit)

- Nephrotoxicity (kidney damage)
- Immunomodulation
- Oxidative stress
- Mitochondrial dysfunction
- Endoplasmic reticulum stress
- Cell death mechanisms
9. Gliotoxin
- Potent immunosuppression
- Triggers cell death in immune cells
- Interferes with NF-κB signaling (crucial for immune function)
- Promotes inflammation
- Disrupts antioxidant systems
- May contribute to multiple autoimmune mechanisms
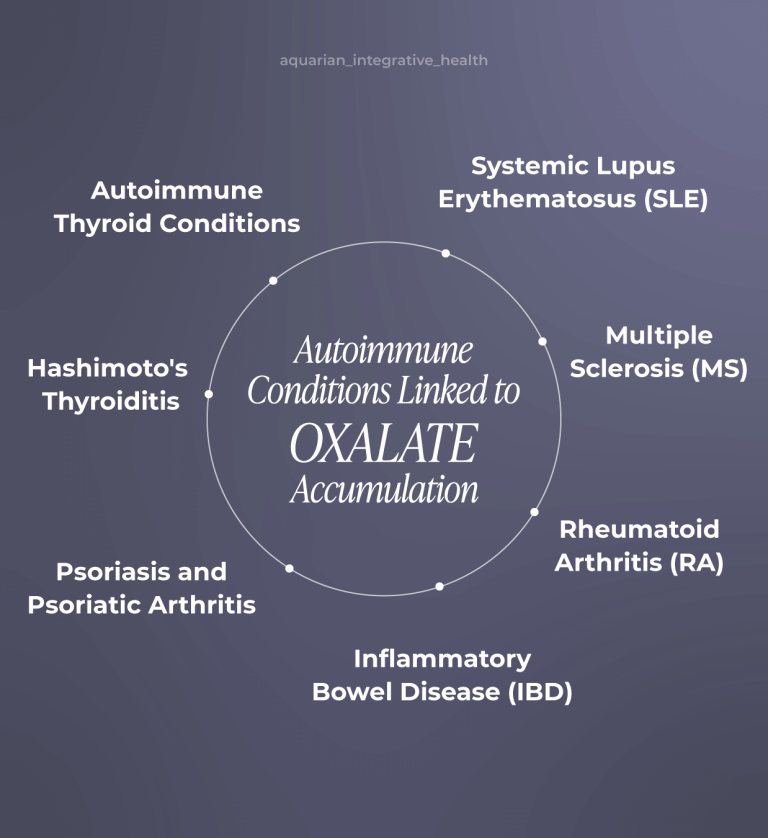
Mycotoxins and Specific Autoimmune Conditions
- Hashimoto’s Thyroiditis: Ochratoxin A is often a trigger for autoimmune thyroid conditions by increasing thyroid peroxidase antibodies.
- Rheumatoid Arthritis: In patients with RA, I see mycotoxin exposure exacerbating joint inflammation and contributing to symptom flares in RA patients.
- Multiple Sclerosis: Due to their ability to cross the blood brain barrier I have seen mycotoxins be a key component in MS as they can damage myelin, the protective covering around nerve fibers that is attacked in MS.
- Systemic Lupus Erythematosus: Many lupus patients that I have seen have mycotoxins as a part of their clinical picture as mycotoxins contribute to immune complex formation and tissue damage characteristic of lupus.
Signs You May Be Affected by Mycotoxins
- Fatigue that doesn’t improve with rest
- Brain fog and cognitive difficulties
- Recurrent headaches
- Joint and muscle pain
- Gastrointestinal issues (bloating, abdominal pain, irregular bowel movements)
- Unexplained weight gain
- Skin rashes or unexplained skin problems
- Increased sensitivity to chemicals and fragrances
- Worsening of existing autoimmune symptoms after consuming mycotoxin-rich foods
Testing for Mycotoxins: A Comprehensive Approach
Comprehensive Mycotoxin Testing Options
1. Urine Mycotoxin Testing
- A provocation protocol (using glutathione, sauna therapy, or ultrasound) before testing can help mobilize stored mycotoxins for more accurate detection
- Hydration status can affect results
- Patients with impaired detoxification may show falsely low levels due to poor excretion ability
- Sequential testing may be necessary to monitor treatment progress
In our office we typically use the The Vibrant Wellness Total Tox Burden test as this advanced panel tests 31 different mycotoxins and goes beyond just mycotoxins to include heavy metals, chemicals, pesticides and other environmental exposures to provide a more complete picture of exposures that may be contributing to immune dysregulation.
2. Blood Markers
In addition to comprehensive urine testing, we leverage specific blood markers to look at the state of the gastrointestinal lining and the overall effect of mycotoxins on the immune system. This often includes markers from the Inflammation and Immune Function Panel:
- Zonulin levels (blood test)
- High-sensitivity C-reactive protein
- Erythrocyte sedimentation rate
- Cytokine panels
- TGF-beta 1 (often elevated with mold exposure)
- Complete blood count with differential
- Immunoglobulin levels (IgG, IgA, IgM, IgE)
- Complement components (C3, C4)
- NK cell function
- Lymphocyte subsets
- Thyroid panel (including antibodies)
- Adrenal function (cortisol rhythm)
- Sex hormone balance
3. Autonomic Response Testing
- Have unexplained fatigue, cognitive issues, or multi-system symptoms
- Show autoimmune markers or diagnosed autoimmune conditions not responding to standard treatment
- Live or work in water-damaged buildings
- Have visible mold in their home or workplace
- Experience symptoms that worsen in certain environments
- Show patterns of inflammation that don’t respond to usual interventions
- Have a history of recurrent sinusitis or respiratory issues
- Present with treatment-resistant gastrointestinal problems
Treatment
Reducing Mycotoxin Exposure in Your Diet
1. Choose Fresh Foods When Possible
2. Store Foods Properly
- Keep grains, nuts, and seeds in cool, dry places
- Use airtight containers to prevent moisture
- Refrigerate sensitive items, especially in humid climates
3. Be Selective About Higher-Risk Foods
- Coffee: Choose organic, high-quality brands that test for mycotoxins
- Nuts and Seeds: Purchase from reputable sources, store properly, and consider soaking and dehydrating them before eating them
- Grains: Opt for fresh, properly stored grains and consider alternatives like quinoa and millet
- Corn and Corn Products: These frequently contain fumonisin and other mycotoxins; my recommendation is to limit regular consumption
Natural Compounds for Mycotoxin Mitigation
Propolis: Nature's Defense Against Mycotoxins
Benefits of Propolis for Mycotoxin Exposure:
1. Direct Antifungal Properties:
2. Mycotoxin Binding and Neutralization:
- Bind to mycotoxins in the digestive tract, preventing absorption
- Neutralize the reactive oxygen species generated by mycotoxins
- Modify the chemical structure of some mycotoxins, reducing their toxicity
3. Hepatoprotective Effects:
4. Immunomodulatory Benefits:
5. Intestinal Barrier Support:
Other Beneficial Natural Compounds for Mycotoxin Exposure
- Chlorella and Spirulina: These algae contain chlorophyll and other compounds that may help bind to and eliminate mycotoxins, particularly aflatoxins.
- Activated Charcoal: An effective binder for many mycotoxins, particularly when taken away from meals and other supplements.
- Bentonite Clay: Has a high binding capacity for aflatoxins and some other mycotoxins.
- Saccharomyces boulardii: This beneficial yeast can help neutralize certain mycotoxins in the intestinal tract.
- Diindolylmethane (DIM): Supports healthy estrogen metabolism, helping counter the endocrine-disrupting effects of zearalenone.
- Modified Citrus Pectin: Binds to toxins while sparing beneficial minerals, making it gentle for longer-term use.
- Silymarin (Milk Thistle): Provides powerful liver support and has been shown to protect against aflatoxin-induced liver damage.
- Curcumin: Offers broad anti-inflammatory and antioxidant protection against mycotoxin-induced oxidative stress.
- N-Acetyl Cysteine (NAC): A precursor to glutathione that supports detoxification of various mycotoxins.
A Holistic Approach to Autoimmunity
- Food sensitivities and allergies
- Gut health and microbiome balance
- Circadian rhythms
- Sleep quality
- Nutrient status
- Hormonal balance
- Additional environmental exposures
Final Thoughts
JUST LAUNCHED
The Autoimmune Revival Method™
The same breakthrough that saved my wife has now helped hundreds of patients break free from chronic fatigue, pain, and inflammation, naturally and permanently.
A Results-Driven Approach to Feeling your Best
Traditional medicine often stops at symptom management, leaving the real problem untreated. Our science-backed approach uncovers the true root cause, treating the whole person to restore your energy, balance, and long-term health.